Monash Medicine in review – Year 1: MED1100/1200
Coming straight from year 12 into university is not a small change. The cohort is much larger, and you may not know many people. You're considered an adult now, and there is a much greater focus on directing your own study.
At the same time, though, medicine is (perhaps unexpectedly) probably the gentlest introduction to university. There is a single cohort of students you spend 5 years with. There are no units to choose from, and the timetable is already prepared for you.
Orientation
The Monash medicine experience begins – online – soon after offers are made. The faculty runs an enrolment information session, running through administrative requirements like mandatory immunisations, police checks and working with children cards.
For students who did not take Biology in year 12, the faculty also offers an online ‘Biology Bridging Course’, which covers basic Biology content. However, the basic biomedical sciences are covered again in the course proper, so you won't be left behind either way.
Simultaneously, the student society, MUMUS, organises ‘Monash Med 20xx’ Facebook groups for each cohort – links are shared in a range of places, including Uni and UCAT DiscussionSpace Facebook groups. The Facebook group connects students for important information and discussion.
In late February comes university orientation week (O-Week), with 2 days set aside for ‘MedStart’, the medicine-specific orientation programme. There are welcomes from faculty members, talks from senior students, and small group activities led by senior students. This was my first clinical skills experience – failing miserably to take another student's blood pressure!
Lunch is organised usually by MUMUS and affiliated groups. See what extracurricular groups might interest you, and don't be afraid to sign up – my time in groups like MUMUS and MedRevue have been responsible for some of the most memorable experiences in medical school.
Talk to the sponsors – typically medical indemnity insurance companies – and sign up for their free medical student offerings. Medical indemnity insurance becomes very important later in life, and it's worth signing up early – even if only for the free merchandise!
The rest of O-Week is yours to make the most of. Come see us at the MUMUS stall and buy some merchandise to flex to family and friends. Sign up for other clubs on camps, and pick up more free stuff. Drop into information sessions at the libraries. If nothing else, drop into Monash University Student Theatre's free O-Show – it's a hoot every year, and I cannot recommend it highly enough.
Semester 1
After the excitement of O-Week comes semester 1 proper – 12 weeks of teaching, plus 1 week of mid-semester break around Easter. The academic component of the course comprises 2 year-long units, MED1100 (a pass-fail-only unit with the formative in-semester assessment tasks) and MED1200 (a graded unit with the summative end-of-semester examinations), all delivered from the main university campus at Clayton.1
The Monash medicine course is divided into four themes:
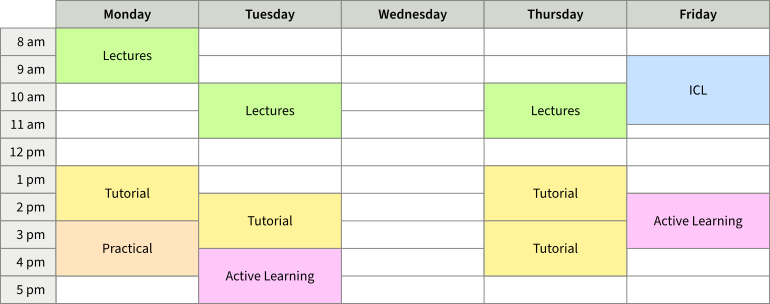
Below is what a typical week in the semester might look like:
The Monash medicine course is divided into four themes:
- Personal and Professional Development. Ethics, medical law, and the self-care/lifestyle-based ‘Health Enhancement Program’ (HEP)
- Population, Society, Health and Illness. Studies in public health and the social aspects of medicine known in semester 1 as ‘Health, Knowledge and Society’ (HKS)
- Scientific Basis of Clinical Practice. The scientific basis of medicine
- Clinical Skills
Didactic teaching is conducted mostly through a few hours of lectures a week, held in the C1 Lecture Theatre, one of the few remaining lecture theatres big enough for the medicine cohort!2 Lectures at the start of year 1 tend to be theme 3 lectures, focusing on basic biomedical sciences – for example, osmosis and body fluids, the biology of cells, and quite a lengthy focus on metabolism. These are accompanied by some theme 2 HKS lectures – introduction to public health – and theme 1 HEP lectures – on lifestyle management and self-care. Lectures are livestreamed, and recorded for later viewing online.
2018 saw the introduction of ‘active learning’ workshop sessions, delivered half the cohort at a time.3 Some of these are didactic-style teaching sessions with some interactivity – frequently on clinical skills, but often on other topics. Others are so-called ‘consolidation’ sessions, done at the conclusion of each block of material, summarising core concepts with revision and quiz questions. These consolidation sessions have been well-received by students.
Throughout semester 1, regular small-group tutorials are held across the various themes, for example, ethics/law/HEP, HKS, clinical skills and occasionally on theme 3 topics. Tutorials – particularly HKS tutorials – sometimes include prereading to do before the session.
Clinical skills tutorials are an area that becomes increasingly important throughout the year. The year begins with the basic principles of clinical skills and development of patient-centred approaches, through to the taking of basic and more advanced histories, and basic procedural skills such as measuring vital signs and giving injections to training models. There is generally even a 1-day clinical placement at a hospital – although at this stage the scope of the placement is understandably limited.
Finally, we have small-group integrated case learning (ICL) tutorials.4 This great exposure to beginning to think about the clinically integrative side of medicine. Each ICL revolves around a case, and is split into 2 parts – part A and part B. Part A covers the initial information about the case. Over the coming week, everyone researches information relevant to the case (e.g. possible causes, how to diagnose and manage, relevant epidemiology), returning next week for part B, covering a discussion of those relevant areas, and part A of the next case.5
In addition to faculty teaching, year 2 students also run optional peer study programmes (PSPs), informal student-led lectures and tutorials, generally on a weekly basis. PSP materials can be very helpful for summarising the key points of each topic and helping prepare for exams
Semester 2
Semester 2 builds on and expands the content of semester 1. Most notable is the introduction of anatomy, with lectures and self-directed learning, beginning with the musculoskeletal and neurological anatomy of the upper and lower limbs.
2 sets of tutorials a week are replaced with small-group anatomy tutorials, historically covering 4 domains:
- Tutorial. Tutorials led by anatomists (usually surgical trainees).6 Generally, the tutorial is divided into groups, and each group researches a particular topic over the week and presents to the group.
- Imaging. Learning anatomy through the lens of medical imaging – at this stage primarily X-rays, CT scans and MRIs, and later incorporating limited other modalities – and gradually learning how to interpret imaging studies. Learning ‘normal’, and then ‘abnormal’.
- Specimens. Looking at and interacting with dissected dry specimens prepared by staff, guided by a workbook with questions to work through. (‘Identify the following structures on the specimen.’ ‘What is the structure marked with a pin? Why is it significant in X condition?’)
- Dissection. Alternately the most dreaded or most anticipated part of anatomy. The bodies of deceased individuals who have donated their remains to the university provides an unparalled opportunity for students to understand anatomy first-hand, in vivo.7 This can undoubtedly be a confronting exercise, but the faculty is aware of this and does well to prepare students.
With anatomy, the final piece of the puzzle in place, the curriculum begins to turn towards a more systems-based approach to teaching. Whereas theme 3 teaching in semester 1 is somewhat of a hodge-podge of miscellaneous basic biology, and theme 4 clinical skills and ICL likewise very broad, the curriculum now focuses in on the musculoskeletal system. Lectures focus on the anatomy of the musculoskeletal system (MSK). Clinical skills tutorials focus on MSK history-taking and physical examination. ICL tutorials cover the assessment and management of MSK conditions.
After the musculoskeletal and neurological systems then comes the cardiovascular system. At last, it is time to bust out the stethoscopes! Exciting!
The curriculum now begins to feel much more integrated, and students typically find semester 2 much more enjoyable than semester 1.
Assessment
Assessment in year 1 comprises a number of formative in-semester assessment tasks, such as written assignments, oral presentations and group assignments, online quizzes and competency-based practical clinical skills assessments.
There are also a number of summative assessment tasks. These include some online quizzes and practical clinical skills assessments, 2 written examination papers at the end of semester 1, and 2 written examination papers at the end of semester 2.
Written examinations are primarily composed of multiple choice questions, though there may be some short answer questions, particularly from themes 1 and 2.
Studying/tips in year 1
For most of year 1, the materials provided by faculty (lecture slides and online materials) are quite adequate. No additional textbooks are really necessary, unless you are keen for more details.
If there is one textbook I'd recommend, it would be Talley and O'Connor's Clinical Examination. While the faculty's clinical skills tutorial notes summarise the key points from Talley and O'Connor, it is an excellent reference text, and one that would serve you well throughout medical school.
The one exception to the above is anatomy. A large amount of self-study is expected in anatomy, and materials provided by the faculty are not sufficient. The recommended textbook is Moore and Dalley's Clinically Oriented Anatomy. Many students also find Netter's Anatomy Flash Cards to be a useful study tool.
One common question from students is ‘Should I buy a stethoscope?’ In semester 1, the only use for the stethoscope is when taking a blood pressure, and stethoscopes are provided, so it's probably unnecessary in semester 1. Semester 2 includes cardiovascular examination, so stethoscopes are useful, but in year 1 generally are provided – although having your own stethoscope will help when practising. The stethoscope gets much more use in year 2, so I'd suggest getting one at least by the end of year 2, and certainly by the start of year 3. By far the most common stethoscope is the Littmann Classic III.
Next: Year 2: MED2100/MED2200 ›
This post revises and updates an old post of mine from 2017. For an account that was a little more contemporaneous, and a little more cringe, click here.
Footnotes
-
Prior to 2019, year 1 was divided into 2 semester-long units: MED1011 and MED1022. References to these units may persist in some outdated documentation. ↩
-
Prior to 2018, medicine lectures were held at R1 Lecture Theatre in the Rotunda, which has since been demolished and replaced by a music precinct and bar. R1 was terrible – you really aren't missing out! ↩
-
The cohort is divided into two groups, group A and group B, which stay the same across years 1 and 2. Tutorial and active learning (except ICL) groups are drawn from these 2 groups, so you end up becoming quite familiar with your ‘half’ of the cohort! ↩
-
Prior to 2018, ICL was known as problem based learning (PBL). But PBL is one of those terms that is used to describe a lot of different things (even later within the medicine course), and so the name was changed for clarity. It appears that before PBL, it was even known as PCL. ↩
-
PBL historically followed this same format. When PBL was reimagined as ICL in 2018, cases were instead completed in the one day, with a 90 minute break for research between parts A and B. In 2020, the format was reverted but the new name stuck. Don't fix what isn't broken, I suppose! ↩
-
Although in one semester my tutorial was taken by a psychiatry trainee! Bless up. ↩
-
However, due to emerging shortages, it has been unclear for some time how long this programme can continue. ↩